Abstract
Introduction: Musculoskeletal toxicities are common in CLL patients (pts) treated with ibrutinib (Ibr) in both upfront and relapsed/refractory (R/R) settings. Importantly, arthralgias/myalgias (A/M) are among the most common reasons for discontinuation of Ibr due to toxicity in reported series (Mato, Ann Oncol, 2017; Mato, Haematol, 2018). Despite this, there are no detailed descriptions and limited guidance for management of A/M.
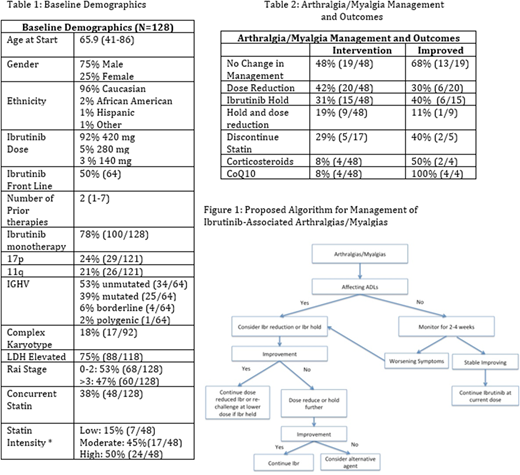
Methods: To characterize this syndrome and its management, we retrospectively analyzed a cohort of 128 pts treated with Ibr at a single academic center from 2011-2017. Demographics, prognostic factors, concomitant statin use, as well as Ibr dose reductions/dose holds, use of NSAIDs/corticosteroids, and the supplement CoQ10 were collected. A/M were graded using CTCAE v4.0 when available, or per physician description as mild, moderate, or severe. Due to clinical difficulty in separating joint and periarticular soft tissue and/or muscle symptoms, we combined arthralgias and myalgias into a single toxicity defined by the most severe grade. Log rank (LR) test was used for comparison of covariates with outcomes. All other statistics were descriptive.
Results: Demographics are summarized in Table 1. The cohort was predominantly male (75%) and Caucasian (95%); 50% received Ibr as front-line therapy and starting dose was 420 mg in 92% pts. 29 pts (24%) had 17p deletions and 26 (20%) had 11q deletions. 48 pts (38%) were on a concurrent statin. 48 (35%) pts developed A/M (20 frontline treatment, 28 R/R). Mean time to development was 349 days (range 7 -1162). 27/48 (56%) developed A/M >6 months from start of Ibr. 39/48 (82%) A/M events were described as mild or moderate (71% Grade 1/2; 19% Grade 3 per CTCAE). 37/48 (77%) of pts had a partial response or partial response with lymphocytosis at the onset of symptoms. 19/48 (39%) pts developed A/M while on a statin. Management and outcomes are described in Table 2. 15/48 (31%) were managed by Ibr hold and 20/48 (42%) by dose reduction; 9/48 (19%) had both. Mean hold duration was 17.5 days (range 2-67). Dose hold was successful in 6/15 (40%) pts, while dose reduction alleviated symptoms in 6/20 (30%); statins were discontinued in 5/17 (29%) pts. Corticosteroids (4 pts) and CoQ10 (4 pts) were used in conjunction with dose holds and dose reductions with symptomatic improvement in 2 and 4 pts, respectively. 4 pts used NSAID or acetaminophen without improvement in symptoms. 2 pts required opiate analgesics for pain management. 29/48(60%) had resolution of A/M during follow up. Overall, no changes in therapy were made in 19 (48%) pts and 13 (68%) had spontaneous resolution of symptoms. Of these patients, 12 had Grade 1 A/M. 40% of pts' A/M persisted, 13/19 (68%) had dose reduction, 8/14 (57%) had a dose hold, 7/16 had both, and 5/19 (26%) had no intervention. Management and outcomes did not differ if A/M occurred before or after 6 months. In this cohort, 46/128 (36%) of pts discontinued Ibr: 11/128 (9%) for toxicity related to A/M; 19/128 (15%) for other toxicity; 10/128 (8%) for disease progression; 5/128 (4%) for transformation; 2/128 (2%) other reasons. Median time to discontinuation of Ibr for A/M was 23.3 mo (1-56.8 mo). Concurrent statin use and statin dose intensity were not associated with increased risk of developing A/M by LR test. Based on our observations, we suggest the following algorithm for the management of Ibr-associated A/M (Figure 1): if A/M do not interfere with ADLs, continue Ibr at current dose and monitor closely for symptom progression, as cases can resolve without intervention. If symptoms affect ADLs, hold or dose reduce until improvement/resolution of symptoms. If managed using Ibr hold, pts can be re-challenged at a lower dose once symptoms improve. If there is recurrence on a lower dose, we recommend observation or consideration or an alternative agent if CLL-directed therapy is still required.
Conclusions: In this cohort, A/M was a frequent event and occurred both as an early or late toxicity, though generally developing after 6 months of Ibr therapy. Dose holds and dose adjustments are the most frequent approach to management, and are the most successful. The role of supportive care agents including corticosteroids and CoQ10 is less clear; however not enough data are currently available to suggest efficacy for any single supportive care agent. Further studies are needed to better understand this toxicity and develop best practice management.
Mato:Celgene: Consultancy; Regeneron: Research Funding; AstraZeneca: Consultancy; Acerta: Research Funding; Pharmacyclics, an AbbVie Company: Consultancy, Research Funding; AbbVie: Consultancy, Research Funding; Johnson & Johnson: Consultancy; TG Therapeutics: Consultancy, Research Funding; Prime Oncology: Honoraria; Medscape: Honoraria; Portola: Research Funding. Kennard:AbbVie, Gilead, Verastem: Consultancy. Landsburg:Takeda: Consultancy; Curis: Consultancy, Research Funding. Dwivedy Nasta:Roche: Research Funding; Incyte: Research Funding; Debiopharm: Research Funding; Merck: Other: DSMC; Celgene: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Research Funding; Takeda/Millenium: Research Funding; Rafael/WF: Research Funding; Aileron: Research Funding. Svoboda:Kyowa: Consultancy; Merck: Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Regeneron: Research Funding; Pharmacyclics: Consultancy, Research Funding; Seattle Genetics: Consultancy, Research Funding; TG Therapeutics: Research Funding; KITE: Consultancy. Schuster:Dava Oncology: Consultancy, Honoraria; Gilead: Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis Pharmaceuticals Corporation: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Genentech: Honoraria, Research Funding; Nordic Nanovector: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal